-
Product Development
-
Clinical Trials
-
Quality
-
GxP Audits
-
Regulatory Affairs
-
Pre-authorisation
- Regulatory Roadmap
- Scientific Advice
-
Product information
-
Dossier preparation
- Dossier Gap Analysis
- MA Handling
- Post-authorisation
- Regulatory outsourcing
-
Pre-authorisation
-
Pharmacovigilance
-
QP Service / Importer
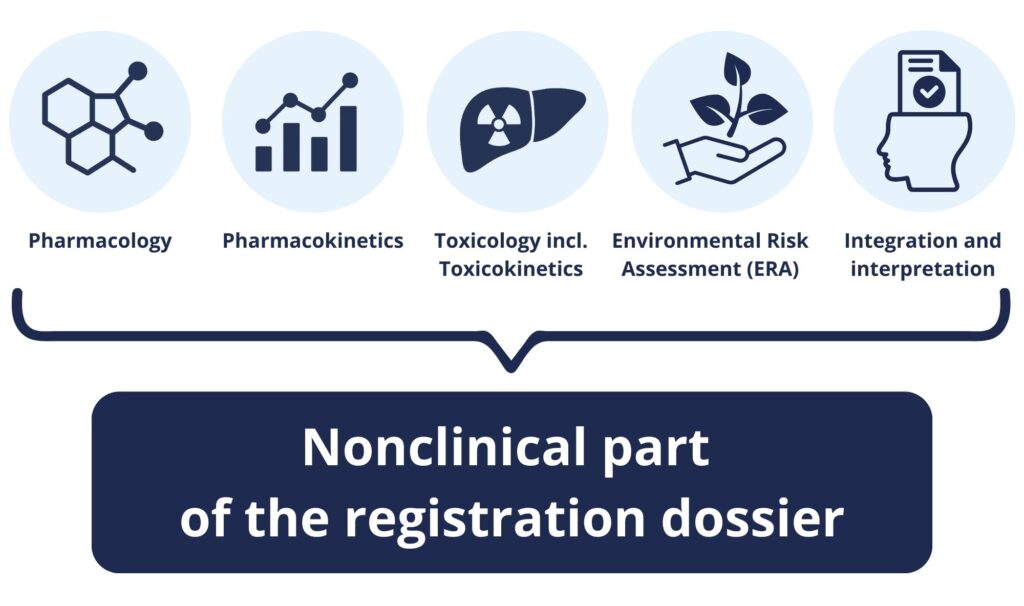
Preparation of the nonclinical part of the registration dossier, nonclinical overview
When submitting a marketing authorisation application (MAA), the Applicant must provide comprehensive data from the medicinal product assessment, encompassing the quality, nonclinical, and clinical parts. The nonclinical component of the Common Technical Document (CTD) focuses on the pharmacology, pharmacokinetics (toxicokinetics), and toxicology of the product, including the active substance(s), as well as excipients, impurities, and degradation products.
Preparation of the nonclinical part of the registration dossier involves collecting and critically assessing the available nonclinical data for the applied-for medicinal product. Data generally comes from the Applicant’s own studies, but may also be supplemented with the results of studies published in the scientific literature.
Our service covers the end‑to‑end preparation of the nonclinical dossier, that is:
- Planning and scoping based on product, indication, route of administration, target population and regulatory strategy,
- Critical appraisal of existing nonclinical data (own studies and literature), including, if planned, justifications for biowaivers,
- Authoring and integration of Module 2.4, so-called Nonclinical Overview, Module 2.6 (Nonclinical Summaries: Pharmacology, Pharmacokinetics, Toxicology), and Module 4 (Nonclinical Study Reports) with cross‑module alignment.
- Preparation of Environmental Risk Assessment (ERA), impurity and elemental impurity qualification, extractables/leachables considerations (where relevant).
- Responses to Regulatory Authority deficiency letters, if such letters occur.
A proper nonclinical evaluation is a foundation for the safety assessment of the medicinal product applied for and an important part of registration success.
What the nonclinical dossier must demonstrate
We focus on the most important: crafting a dossier that convincingly supports your product’s safety profile, indication(s), dosing regimen, and risk management.
Pharmacology
- Primary and secondary pharmacodynamics: mechanism of action, on‑target and off‑target effects; relevant safety pharmacology (cardiovascular, including QT, respiratory, CNS).
- Justification of pharmacological models and translational relevance to the target indication.
Pharmacokinetics / Toxicokinetics
- ADME characterisation – systemic exposure in key species, mass balance/metabolite profiling, comparability of exposure between animal species and humans.
- Interspecies scaling, identification of major metabolites (and relevance to humans), drug‑drug interaction potential (nonclinical).
Toxicology
- Single‑ and repeat‑dose toxicity: organ toxicity, dose/exposure-response, NOAEL derivation, margins to clinical dosing.
- Genotoxicity (in vitro and, if applicable, in vivo justified sets) and carcinogenicity (per ICH S1 strategy, including weight‑of‑evidence when applicable).
- Reproductive and developmental toxicity (male/female fertility, embryo‑fetal development, pre/postnatal), lactation considerations.
- Local tolerance, phototoxicity, immunotoxicity, sensitisation (where relevant).
- Excipient safety
- Toxicology of impurities.
- Toxicology bridging for changes in route, strength, or formulation (including extractables/leachables for inhalation, parenteral and device‑combination products).
- Juvenile animal studies (ICH S11) when paediatric use prompts a dedicated assessment.
Environmental Risk Assessment (ERA)
- Phase I/II evaluation: risk characterisation, and proposed risk‑mitigation measures where needed.
Integration and interpretation
- Comprehensive, balanced discussion of benefit–risk in the intended populations.
- Clear identification of knowledge gaps, uncertainties and risk minimisation measures (e.g., labelling statements, RMP cross‑references, post‑authorisation commitments).
- Robust consistency across Modules 2, 3, 4 and alignment to clinical strategy (Module 5).
Our approach by application type/strategy
We tailor the nonclinical documentation to the type of application and regulatory strategy:
- Original products – full nonclinical program aligned with international guidelines.
- Generics and hybrids – focused on bridging data and justifications for waivers.
- Well-established use (WEU) – literature-based summaries supported by risk assessments.
A well-prepared nonclinical section is essential for demonstrating that the product can be used safely and effectively. It supports the overall benefit–risk assessment and helps avoid unnecessary regulatory questions during review.
Why us?
We provide comprehensive registration services with seasoned nonclinical and clinical regulatory expertise. Our team brings many years of experience with authorities and scientific advice, ensuring fit‑for‑purpose nonclinical strategies that minimise unnecessary studies, while satisfying regulatory expectations.
Benefits of cooperation
- End‑to‑end support. We can prepare the nonclinical documentation together with quality (Module 3), clinical (Modules 2.5, 2.7, 5) and product information (SmPC, PIL, labelling), and then manage the entire registration process.
- Regulatory efficiency – we routinely anticipate and avoid avoidable authority questions. If they arise, we lead the dialogue and propose pragmatic solutions, which include post‑authorisation commitments where appropriate.
- Integrated risk management – nonclinical conclusions translated into clear labelling and RMP alignment, which ensures coherent, reviewer‑friendly dossiers.
Do you need assistance with the nonclinical part of your registration dossier or full regulatory support? If so, please get in touch with us so we can discuss your needs and develop a strategy that ensures compliance and efficiency.